- Chembur, Mumbai, 400071
- +91 9136113321 | +91 9930553321
- drsheths@gmail.com | itsdr@hotmail.com
- Mon to Sat: 4pm to 8:30pm
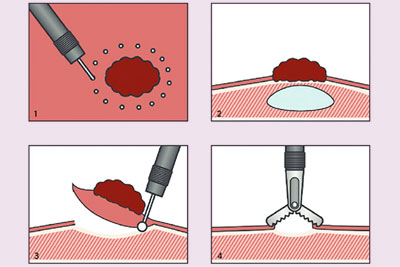
Endoscopic Submucosal Dissection (ESD) is an advanced, minimally invasive endoscopic technique used to remove large or high-risk precancerous lesions and early-stage cancers from the gastrointestinal (GI) tract, including the esophagus, stomach, colon, and rectum.
Unlike standard polypectomy or Endoscopic Mucosal Resection (EMR), ESD allows for en bloc (single piece) removal of deeper and more complex lesions with greater precision, reducing the risk of recurrence and enabling accurate histological assessment.
ESD is primarily indicated for:
ESD is safe when performed by trained specialists. As it is technically more demanding than standard procedures, it may carry a slightly higher risk of:
However, most complications are rare and can be managed during the procedure itself.
ESD is a cutting-edge technique offering curative treatment for select early cancers and advanced lesions of the GI tract—avoiding the need for major surgery while preserving the function of the digestive system.